I cannot stress enough the importance of maintaining a solid, consistent bedtime schedule. If your child or client has already developed bad habits in this area, this will be much harder to combat. But if you stick to your routine, eventually the child will learn to look forward to bedtime.
Within this podcast episode and video blog, I discuss simple changes that can make all the difference.
You’ll Learn:
- How to assess sleep habits
- How to create a healthy bedtime routine
- Why only one parent should carry out bedtime preparations (bathing, brushing teeth, putting on pajamas, bedtime story, etc)
- Reinforcements to help your child stay in their own bed
I will also provide several valuable resources that are packed with great information on creating a healthy bedtime routine and sleep patterns. This includes three books by reputable authors, as well as my own Ebook that you can now download for FREE.
Autism and Sleep Problems
Poor sleep is very common in children with autism. With my own son, Lucas, I struggled with getting him to sleep in his own bed through the night for ten years. Using ABA techniques though, I was finally able to establish step by step procedures that resulted in him sleeping through the night consistently in his own bed. That’s why I want to talk all about autism and sleep, and what you can do to stop playing musical beds and get more quality sleep for both your child and yourself.
When I was writing my book in 2006, Lucas was nine years old and I remember my husband saying “whatever you do don’t put anything about sleep in your book because you have no idea what you’re doing when it comes to autism and sleep.”
By this point, I had been a BCBA for three years and had already worked with hundreds of children through a statewide grant in Pennsylvania. But my husband was right. I was very bad at shaping up good sleep habits with my son, Lucas.
Every night, despite giving Lucas melatonin and starting him out in his own bed, he would wake up. He sometimes would be up for hours, but oftentimes he would run in our room and climb into our king size bed and fall back to sleep. Sometimes I would end up in his bed and sometimes he would end up in our bed. But for the first 10 years of Lucas’ life, we dealt with disrupted sleep patterns every single night.
Providing Special Reinforcement
I took my husband’s advice and didn’t put any autism and sleep information in my book. It wasn’t until a few years later when I went to give a full day presentation in Ohio that I met a BCBA who specialized in sleep. She helped me with a few key pieces of information regarding sleep.
One of the first pieces of advice was for me to lock our bedroom door at night. This prevented Lucas from just barging in and jumping in our bed. I explained to Lucas that the door would be locked and he would need to knock. I also explained that he would get a special reinforcement for sleeping in his own bed and for waking up alone in his bed in the morning.
For Lucas, this reinforcement was a special kind of cookie that he wasn’t going to get for anything else. You might be thinking “my child won’t understand all that,” but I didn’t think Lucas would either at that point.
So I picked a date, locked my bedroom door, and when Lucas would knock I would return him to his bed and tell him that he needed to sleep there for the special cookie in the morning. This offer of reinforcement was key to preventing problem behaviors that may have occurred.
The first night he woke up three times. Each time I returned him to his bed and reminded him that he needed to stay in his own bed alone for the special cookie in the morning. The second night Lucas woke up twice and the third night just one time.
The fourth night – after 10 years of struggling with sleep – Lucas slept in his own bed through the night.
Getting Help for Autism and Sleep
I went on to help many children with autism sleep through the night in their own beds. A lot of times it takes a little bit more time than just three nights and several more interventions and database decisions. And children could have other sleep problems like sleep apnea. Sleep is just like any other behavior, it can be shaped and it can be changed and it can be improved through the science of applied behavior analysis.
Sleep is a necessity no matter how you spin it. If your child doesn’t sleep through the night, then neither will you. Knowing what I know now, I wish I would have fought to regain my sleep much sooner. I implore you to not make that same mistake and allow me to help you create a bedtime routine. It will lead you to live your happiest, most well-rested, life. To learn more about resolving sleep issues in children with autism, make sure to claim a copy of my free eBook “Stop Playing Musical Beds”.
Mentioned in this episode:
— Get Your Free Sleep Ebook
— MaryBarbera.com/workshop (Sign up for a free online workshop for parents and professionals)
— Sleep Better!: A Guide to Improving Sleep for Children with Special Needs, Revised Edition, by Mark Durand Ph.D.
— Sleep Difficulties and Autism Spectrum Disorders: A Guide for Parents and Professionals, by Kenneth Aitken
— How To Get Your Child To Go To Sleep And Stay Asleep, by Kirsten Wirth

Transcript
You’re listening to the Turn Autism Around podcast. In this episode, I’m going to be discussing sleep problems and children with autism. I’m pretty sure you probably know that kids with autism have more sleep problems than typically developing kids and often have trouble falling asleep, sleeping alone, staying asleep and not waking up before the crack of dawn. So it’s an important issue for both parents and professionals to learn proven strategies to get kids sleeping better.
Before we get to the information, I’d like to give a shout out to one of our listeners who gave the podcast a five-star rating and review on iTunes. This is from Restart Runner who said, “this podcast is a must listen to for parents of a diagnosed child. In fact, all of Dr. Barbera’s resources, her bestselling book, videos, and now this podcast help navigate the autism maze, which is brutal, confusing and overwhelming. Dr. Barbera helps provide insight to those looking for answers.” And I have to agree with Restart Runner, thank you for that review, and I have to agree that the autism maize is often confusing, overwhelming, and I haven’t ever described it as brutal, but in many situations it is. And so I am hoping to help people navigate that maze with a little more ease. So let’s get to this episode all about sleep.
Welcome to the Turn Autism Around podcast for both parents and professionals in the autism world who want to turn things around, be less stressed, and lead happier lives. And now your host, autism mom, behavior analyst, and bestselling author, Dr. Mary Barbera.
Hi and welcome back to another episode of the Turn Autism Around podcast. I’m your host, Dr. Mary Barbera and I’m thrilled that you are here with me. As you may or may not be aware, sleep is a really complicated issue, especially for children with special needs and autism. Many children have difficulties falling asleep like my son, Lucas. I’m going to tell you some more details about his sleep problems, especially early in life, and because of kids having difficulty falling asleep, sleeping in their own bed, I often say that many families are experiencing a bad game of musical beds.
And I wrote an Ebook about sleep called Stop Playing Musical Beds: Solving Sleep Problems in Children With and Without Autism. And we used to sell it for $10, I think. And now we are for the first time ever, we are giving that away for free. So I encourage you to keep listening but check out the show notes or you can just go to marybarbera.com/sleep and you can download your free Ebook, which I’m going to be giving some highlights about how to use the Ebook and some proven strategies that I’ve learned over the years and use. So I hope that you will get that free resource when we’re finished.
So as you probably know, if you’ve listened to other podcast episodes, if you haven’t, welcome to this episode, it might be helpful if you go back to the first episode and learn more about my journey. But, um, which is marybarbera.com/one but just to recap, I’m the mom to two boys, Lucas and Spencer. And Lucas was diagnosed one day before his third birthday, but he did have a regression about 15 to 18 months of age. He started to regress in some areas, but I was pregnant with my second son, Spencer, and I wasn’t really concerned about development. I didn’t know much about development. And I kind of missed a lot of the first signs of autism. I also was in big time denial when my husband first mentioned the possibility when Lucas was just 21 months old. So I spent a year like our reviewer said, you know, in an autism maze in denial, very overwhelmed, very confused. And both of my boys are young adults now, but both of them had some sleep issues that caused a lot of turmoil in our family when they were young.
So since Lucas regressed, he had more difficulty falling asleep. He never was a great sleeper though. Neither of my boys were great sleepers. I would find myself taking them for a ride. They were only 18 months apart. So it was really like critical that they sleep kind of at the same time. They weren’t, you know, I wasn’t a behavioral analyst back then so I really didn’t know how to get my kids to fall asleep in their cribs for a nap. I didn’t have the routine that they needed.
So I used to take them on sleepy drives and, you know, just caused a lot of problems because Lucas especially would wake up in the middle of the night… When he was diagnosed a day before he was three, we were having significant sleep problems and the developmental pediatrician recommended Melatonin, which is a natural supplement. You can get online, you can get over the counter. And while back two decades ago Melatonin wasn’t really a proven treatment for sleep, especially for kids, it was kind of off label. But the doctor did recommend it and we have found… Lucas is still on Melatonin. Many of my clients were also on Melatonin based on their physicians telling them to try it.
Oh, before we go too much farther, I do want to say as a behavior analyst and a registered nurse, I just want to be clear that when I throw out strategies that I’ve used or strategies that, like especially Melatonin or other supplements or medications, but even behavioral treatments like putting a gate at the door of their bedroom or… Please know that these are not, this is not clinical advice. This is not medical advice for you. This is not behavioral advice for you because when you treat behaviors, whether you do nothing or whether you put a gate at the door or give Melatonin things can backfire, and depending on your situation, they could backfire in a big way. So all of the information I provide is not a medical or behavioral advice. It is just for informational purposes only. Really to make the most headway you need a qualified medical and or behavioral professional who can assess your child, make a plan, and help you intervene the best.
But unfortunately, many parts of the world and many parts of the United States, we just don’t have the type of person that can come in and really help you. You know, there are waiting lists, there are copays, there are private pay situations. And what I hope to do through my podcast and my video blogs is give you practical strategies that you might be able to use. You might be able to read books or you could join my online courses and community for more in-depth information and dive deeper into this. But, so I just want to, as I’m saying, Melatonin and many of my clients were on Melatonin, I mean that was never recommended or prescribed by me. It was always like, check with your physician and see if Melatonin might be a good choice for you.
So, when Lucas was two until he was 10, he never slept in his own bed throughout the night. We played constant musical beds in our house on most nights. If Lucas would… He would always get Melatonin and he might fall asleep, but then he didn’t stay asleep. And if he woke in the middle of the night, say he woke up at two in the morning, he would run in our bed, sometimes jump in our bed, and sometimes I could get if I just didn’t move, he would fall back to sleep. If he started stemming or started making noises in his own bed, if I would go in there, you know, it could be two to five in the morning where we were both up and he was kind of really hyperactive.
I mean there was just different, different things went on different nights and it was confusing. But my husband was and is an emergency medicine physician so he had to sleep, and I was home with the kids during the day. So weekdays or if my husband had to work the next day, you know, it was pretty much me trying to get Lucas to go back to sleep. Cause I’m the kind of person that really needs sleep and we all need sleep, and I think a lot of parents of kids with autism are really sleep deprived. But I found that the odds of us staying up and having to monitor him for hours on end were much greater if I went to his room and you know if I let him jump in our bed, I had a had chance of him falling back to sleep. But this whole musical beds shaped up very poo sleep behavior in our house.
Spencer was pretty good about falling asleep and staying asleep in his own bed after he got to be two or three years of age. So he was in his own room. Thank goodness that he didn’t have to share a room with Lucas cause that would’ve really been a problem. But since, as I said, I didn’t work outside the home, I pretty much was trying to tackle this. But you know, when Lucas was six or seven, I became a behavior analyst back in 2003, and even as a behavior analyst, we had shaped up such bad sleep in our home that I really wasn’t able to have an objective view to try to fix our sleep problems. And when I was writing my book Lucas was about nine I think, and this is back in 2006, and I had been a behavior analyst for three years, I’m writing my book and my husband looked at me one day and he said, whatever you do, do not put any advice about sleep in this book because you are terrible at sleep. And he was right. And if you look through my book, The Verbal Behavior Approach, which has sold more than 50,000 copies, it’s in 12 languages, there is not one advice about sleep.
However, shortly after my book was published in 2007 I did go to many places and started speaking about the procedures in my book. And one of the speeches that I gave was a one day talk in Ohio. It was one of my first speaking engagements after my book in 2007 I believe, and a behavior analyst, and I’m sorry, I don’t even remember her name, but she was a behavior analyst. She took me out to dinner the night before I spoke, and we were chatting about Lucas and I told her about his language and potty training and all that stuff. And she asked me about his sleep, and I told her that I wasn’t good at sleep, that that’s why there was not any advice about sleep in my book. And she basically told me she was an expert at sleep and she was a behavior analyst. So she was basically shaking her head thinking, Oh God, this woman just wrote a book and she has no idea what she’s doing with sleep. So she gave me really good advice just at dinner, you know, just things I could try to get Lucas to sleep in his own bed.
So basically she said, and Lucas is 10 at this point and he was well over a hundred pounds. He was a big 10-year-old. So it was coming to the point where he would barge in our room, jump over me to get to the middle of the bed. And I was like, I’m going to get like, you know, accidentally injured by this because I’m like sound asleep. And all of a sudden a hundred pounds come like pummeling towards me. So she basically said we needed to prevent Lucas from entering our room by locking our bedroom door and that was going to be the only way we could get him to not get in our bed. Because once he was in our bed, now it’s nighttime, now I’m startled. Now he’s comfy in the bed and that’s what he’s used to.
So she also said that he should not have a TV in his bedroom, but he had already had a TV in his bedroom for 10 years; that was the way he fell asleep. And so I didn’t take her advice about the TV. I left the TV in the room figuring, okay, I’ll leave the sleep in him falling to sleep is the same. And I’m just gonna start with, I’m gonna lock my bedroom door and I’m going to tell Lucas, like, I’m gonna lock my bedroom door and you’re going to have to knock or you know, just try to open the door and then Mommy’s going to walk you back to your bedroom, and in the morning you’re gonna get a special treat.
So now many parents would stop at this point, because this is in my free Ebook, which you can get at marybarbera.com/sleep, and many parents would stop and be like my child’s too… they’re not understanding all this language about the treat in the morning or anything like that. I would have to say that Lucas didn’t really understand that either. And we practice a little bit with me locking the door and him knocking or you know, jostling the handle. But kids don’t really need to understand like everything.
And in some cases, like we would have had to put a gate at the steps or… I don’t like to gate kids rooms if they’re potty trained because they may have to get up to use the bathroom in the middle of the night. So we didn’t get his room and he had never been known to walk down the stairs, so we didn’t need to gate the stairs. We just needed to lock our bedroom door. And the first night of the intervention I planned, okay, these next three to five nights might be tough. He might get up 10 times and I might have to walk him back 10 times. I didn’t know what was gonna happen.
But the first night he woke up three times he came over, knocked or jostled the handle. I got up, unlocked the door, said, Lucas, you’re going to get a special treat in the morning, I named it, we’ll just say it was a cookie. And so you’re gonna get a cookie in the morning. You need to stay in your own bed. Mommy’s going to help you get back in bed, get back in bed, covered him up, kissed them, walked out, closed his door, went back into my room and I fell back to sleep. He came in the second time and the third time that same night, and I jotted down, I just looked at the alarm at the clock and I jotted down the three times he woke up. He didn’t have any problem behaviors. He didn’t cry when I left the room. So the first night, it was three times he came over, the second night he woke up and came over just twice. And the third night of intervention he woke up just once, came over, knocked and returned and got his special treat in the morning. And then by the fourth night, he never came over again.
And as a behavioral analyst, I was thrilled that the intervention worked so well. It was just a beautiful thing. It was a beautiful graph: three times the first night, two times the second night, one time the third night. And we are done with sleep problems and him jumping in my bed. But I was also kicking myself because I let this behavior go for 10 years without tackling it. And it would have helped Lucas learn to fall asleep, you know, when he was five or stay in his bed, it would have helped our family sleep hygiene. It would’ve helped so much if I would’ve tried this a little sooner. So that’s why I now, you know, I’ve helped dozens of my clients and children of the parents and professionals that are in my online course and community. I’ve helped them just by telling my story. Just by telling people that you don’t have to deal with these horrible sleep issues for the rest of your life. It’s not a part of autism, it shouldn’t be a part of autism, and we can treat it.
And there are people that have worse problems. Like I’ve consulted with families that with 20-year-olds who are literally the parents are sleeping on a mattress on the floor because they’re afraid their child’s going to leave the house or burn the house down, and there are huge safety issues.
So where do you start? And obviously, with a short podcast, I’m not going to be able to give you every piece of information about sleep. And that’s why I encourage you to get the free sleep Ebook that I wrote at marybarbera.com/sleep. But I do want to give a shout out to three books, three authors that wrote books that help me in my quest to help others because while I got the advice from that one behavior analysts in Ohio, and if that person is listening, please email me and let me know what your name is. I am just completely blanking on that. But okay, so there are three books that I would recommend.
One book is by Dr. Mark Durand and that is called Sleep Better. He’s a worldwide expert on autism and sleep and he wrote his first edition of Sleep Better in 1998 and I think it’s really a comprehensive book and it’s a classic book on sleep. And the second edition was written in 2013.
Another great book was published in 2012 called Sleep Difficulties And Autism Spectrum Disorders, and I found this book particularly helpful for all the research that has done on sleep with children, specifically with autism. It’s quite comprehensive and it also has seemed to have more medical information like about Melatonin for instance, that I didn’t find at least in the first edition of Dr. Durand’s book.
And the most… another more recent book is published in 2014, and it was published by behavior analyst Kirsten Wirth, and she has a Ph.D. and she wrote, How To Get Your Child To Go To Sleep And Stay Asleep. This is not specifically for children with special needs, but there’s a lot of advice for typically developing children which with a lot of anecdotes of Kirsten’s personal situation with our own children. And her book, Dr. Wirth’s book, has some interesting statistics that sleep disorders are common in all children in that 15 to 40% typically developing children will have some sleep disorders at some time in their life. And children with special needs have sleep disorders at a rate of about 85%, so you’re not alone if you’re a parent out there with a child who has sleep issues.
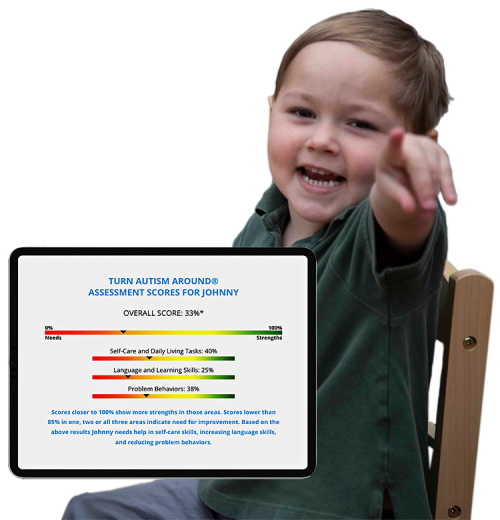
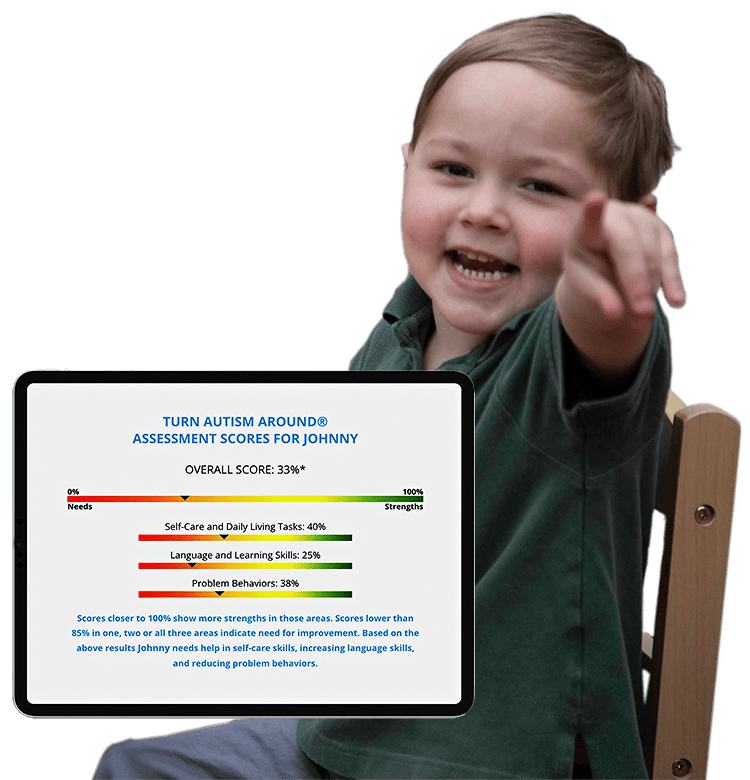
And even if you’re a professional, the parents really need your help and some guidance, and even pointing them towards this Ebook and this podcast might be a great start. So where you start with any issues, so in this case, sleep is you have to start with an assessment and that doesn’t have to just jump into sleep. We should be doing a quick assessment of the whole child because if a parent comes to me and says, my child is a horrible sleeper, I’m gonna want to know more information like the child’s age, their ability level, their language level, can they walk, are they potty trained? You know, those sorts of… Do they leave the second floor if they’re, you know, do they leave the home, are they safe wandering around the house? You know, are they safe in their bedroom?
So we need a little bit more information than just sleep. But one of the first things that I think professionals sometimes miss is instead of just diving into the child’s sleep issues is we need to assess the parent’s concern about sleep issues. Are the parents struggling with the child’s sleep? I was really struggling. I was really tired of our sleep situation. But I had a family, a client from a family in India for instance, and they, I mean they were living in the United States but they were from Indian culture and in India, it’s quite common for children to co-sleep with their parents until an older age. So they weren’t really struggling with sleep and they didn’t really want to intervene. So, but if sleep is a big problem on the top of the list for families, then the parents’ motivation to change the sleep will be an important factor.
So assuming that the parents are having problems with the child’s sleep and want to intervene in some way, then it’s time to really assess the child. I do have a one-page assessment and then my online courses and community, we use the VB-MAPP as a basis usually. I do have some additional assessments, but we want to go deeper into assessment and not just about sleep. In many situations though, when we are really just talking about assessing sleep, we want to interview the parents and talk about like, where does the child fall asleep? Where does he sleep? Where do you want him to sleep through the night? Where does he sleep currently? In many situations when the child’s not sleeping well, they’re falling asleep on the sofa and being carried up to bed. You want to know what the whole bedtime routine looks like.
Are they getting a bath or a shower? Are they returning to the kitchen or the family room to watch TV or for a snack? Is the parent reading them a book? Is the parent laying in a twin bed with the child? Do the parents sit on the floor in the child’s room? Do they just all sleep in the same bed, but that’s not ideal? Does the child, like I said Lucas and Spencer did not share a room. Do they have to share a room with a sibling? Are they in a bunk bed? Are they on the bottom bunk? Are there five children in the house and three of them share the same bedroom with a child with autism? I mean just a lot of factors that could be important in terms of making a plan. We have to step back and look at the whole situation.
And also ask about naps because this can often detour the whole bedtime routine. It’s almost like if a child takes a nap, especially a late or long nap, then the child’s body resets. And so for kids older than two or three, I really don’t think napping is a great idea unless the child has to get up for daycare or something at an extremely early hour, then a nap may be necessary. But if a child’s having problems falling asleep at eight or 9:00 PM but they’re getting a nap at three, three to 5:00 PM, then there’s probably your problem.
Okay. Some other questions to ask in the assessment. How long does it take for the child to fall asleep? How much sleep does a child end up getting? What time do they nap usually? Start, stop. Do they nap in a crib or bed or do they take sleepy drives or do they nap on the sofa watching TV? What time would you like them to go to sleep and get up? Also, you want to assess are they using a pacifier, or is there a special blanket or something that they need to fall asleep or stay asleep?
In terms of naps, especially as the child gets older, we want to limit naps in terms of duration. Most experts say that a child should not be sleeping after 3:00 PM or nap. And if the child falls asleep at three like I said and naps until five they’re going to have problems falling asleep at eight. We also don’t want naps to extend past an hour or an hour and a half max, sometimes even shorter. And we want to make sure that these naps are all finished by 3:00 PM.
Okay. So then you also want to assess what happens if and when a child wakes during the night as Lucas did. Does he come to your bed? Does he scream? Does it go to the gate? Is the door gated? There are lots of things. We also want to assess what’s in the room; Is it safe? Are there dressers bolted to the walls? So if a child is climbing they won’t get hurt by having the dresser actually fall on them. I do know of a situation where a child died in that situation where, I don’t know them personally, but the dresser did fall on the child and pinned the child and killed the child. So we want to make sure that, especially if the child is waking during the night, that we make sure that they’re in an as safe condition as possible. So once we do a full assessment, whatever that entails, we need to make a plan and the plan has got to involve the parents, the caretakers, because if they’re not willing to carry out the plan, it’s not going to work.
So like I said, you want to stop or decrease naps. You also want to take a look at multivitamin supplements or anything late in the day or caffeine that could affect things. Also, liquids after dinner time… sometimes children wake because they have to go to the bathroom or if they’re not toilet trained, you do want to check their diaper when they wake up because they might be waking up because they’re wet. So you want to limit that liquid intake after dinner. And you also want to limit spicy food, fatty food, things that might upset the child’s stomach. If you can wean from pacifiers if at all possible. I do have a blog on how to wean from a pacifier, as well as a free cheat sheet about the steps to wean from passive and bottles.
If there’s not currently a TV in the room, I’d highly recommend not putting one in there in the bedroom. Bedrooms should mean sleep, not running around the room, wrestling with the parents, tickling, watching TV or playing with their iPad. But if you already have a TV in the room and it’s working at least to get the child to sleep like it was for Lucas, you may want to consider leaving it in there temporarily. I do find that having a TV with a remote control and a sleep timer is better than an iPad, but you know there are all kinds of things that are going on with our kids and sometimes you just have to pick the plan that you think is going to work best.
If the parent’s goal is to have their child sleep through the night and they’re in their own bed, which I believe should be the goal in most cases, you need to do an assessment which would help improve the bedtime routine, which may include the child’s needs to fall asleep and stay asleep in their bed alone.
I do know of many families who have the child falling asleep on the sofa and then carrying the child upstairs, and even if the child is three or four years of age and you can physically do it, it’s going to be impossible as the child gets older. And so I would really recommend that you take a look at the Ebook and try to get your child into a routine that involves, like, bathroom, shower or bath, brushing teeth, and then to bed; not returning downstairs to watch TV or returning downstairs for a snack. I think that gets us into trouble. And if the child needs an adult in his room at the moment to fall asleep, I would suggest that the parent sit on the side of the bed, sit in a rocking chair or even put a cot or a trundle bed somewhere where you can fade yourself out of the situation as easily as possible.
Part of the plan also needs to include what kind of reinforce you’re going to use because children, you know, the behavior will go up if it’s being reinforced and sometimes praise and stickers is just not going to cut it.
The final thing I’ll say is the bedtime routine really does need to be a list of things in the order. So if dad, when he helps put the child to bed, has them brush their teeth and then has them go to the bathroom and then has them put their pajamas on, but mom is first bathroom, then tub, then you know, if you do it out of order, the child’s not going to have this nice stable routine. So in many cases, I do recommend that one parent is really the one that takes the lead on the bedtime routine until you can get it figured out.
In my case, it only really took three days. I mean, we had a bedtime routine, but it only took three days to stop the nighttime waking. So hopefully you can make a plan that works as quickly as that, and then you’ll be golden. And then how do you keep track of all this? And in my free Ebook, which is marybarbera.com/sleep, I give you some ideas about how to take data. And in some cases, you know, like Melatonin for one of my clients, it made her more hyper and more likely to wake up during the night. And for her we just needed to stop the multivitamins towards bedtime. And that was big too.
So I do have a technique to use a calendar to keep data and I do find that that’s really a great thing that you can… on a calendar. Usually, a paper calendar is, you know, the nap time start/stop the bed time at nine o’clock, but they didn’t fall asleep until 9:30, 10 o’clock. And then they woke up at two in the morning and then they fell back to sleep at three in the morning and then they slept till seven in the morning. All of this data is really important and we want to get to the point where the child is tired when they go to sleep, and the child hits the pillow and falls asleep pretty quickly because if they’re laying in bed or they’re getting out of bed and running around the room,that’s not going to shape up really good flow in terms of getting the child to fall asleep and stay asleep in their own bed.
So just to recap some big mistakes I see with sleep are not dealing with naps that are too long and too late; giving multivitamins or any caffeine or any kind of foods that would upset the stomach, or even a lot of liquids at night, which can cause nighttime waking; being inconsistent with that bedtime routine; returning to the kitchen or the family room or in the middle of the bedtime routine; letting kids fall asleep in cars or on sofas and then carrying them up to bed. Those are all some of the some of the most common sleep problem.
So I’m really hoping that I’ve given you some strategies, some information that might help you, whether you’re professional and you can help a lot of parents with their sleep issues, or if you’re a parent yourself struggling with sleep, I encourage everybody to go and download my free Ebook now available at no cost at marybarbera.comsleep and I hope that you tune in next week. Don’t forget, if you love this podcast to go to iTunes or wherever you’re listening, leave me a rating and review and I’ll catch up with you next week.
Thanks for listening to the Turn Autism Around podcast with Dr. Mary Barbera. For more information, visit marybarbera.com.